

-
Meet Sue
-
Further Data - Sue
Case Study

One cardiovascular event a year ago AND in the last
78 months diagnosis of PAD in another vascular bed
LDL-C 5.1 mmol/L currently treated with atorvastatin 40mg
ESC/EAS target 1.4 mmol/L AND ≥50% reduction from baseline;1
NICE PCSK9i eligibility threshold ≥3.5 mmol/L2
NICE lipid target: 2.0 mmol/L or less3
Case Study
Potential LDL-C reductions from baseline
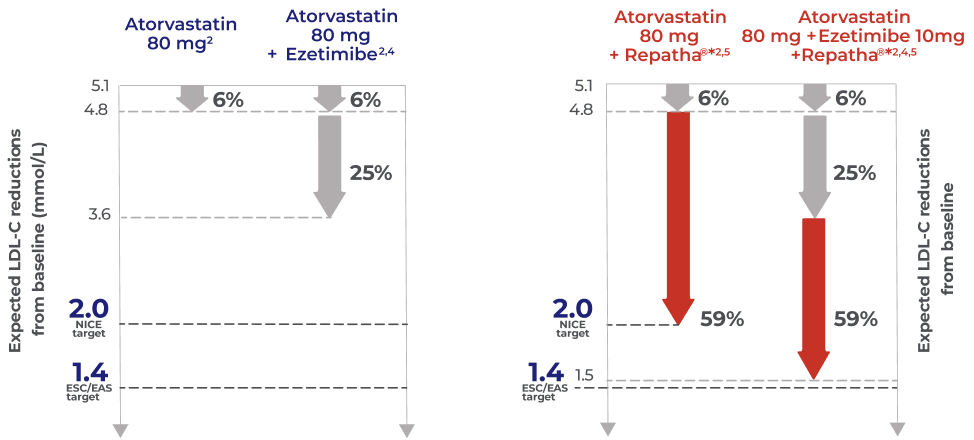
The expected LDL-C reduction and LDL-C levels between treatment regimens are not comparable and are for illustrative purposes only. High intensity statin: atorvastatin 40mg or 80mg daily. Ezetimibe monotherapy: Ezetimibe 10 mg daily. High statin monotherapy and ezetimibe: Atorvastatin 40mg or 80mg daily, and 10 mg ezetimibe daily. Repatha® monotherapy: Repatha® 140 mg bi-weekly.
*In the FOURIER trial, 59% LDL-C reduction was achieved with Repatha® in addition to high-or moderate-intensity statin therapy vs statin + placebo
-
Meet George
-
Further Data - George
Case Study
One cardiovascular event and statin intolerant
LDL-C 5.2 mmol/L on no treatment
ESC/EAS target 1.4 mmol/L AND ≥50% reduction from baseline;1
NICE PCSK9i eligibility threshold ≥4 mmol/L2
NICE lipid target: 2.0 mmol/L or less3
Case Study
Potential LDL-C reductions from baseline
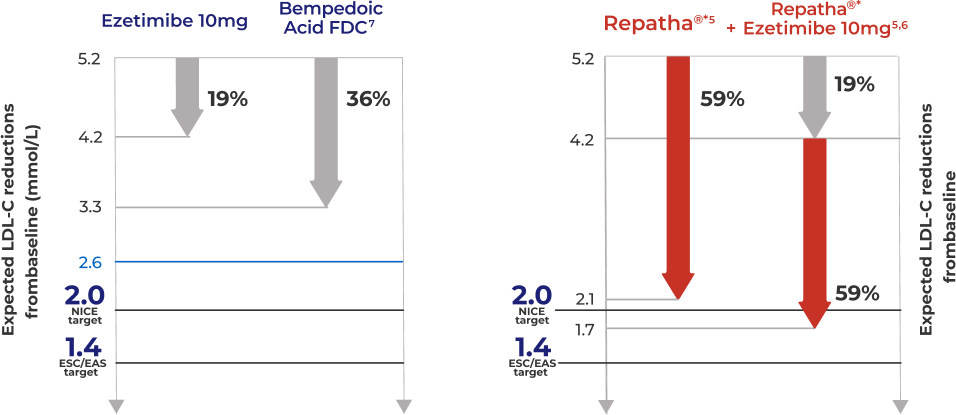
The expected LDL-C reduction and LDL-C levels between treatment regimens are not comparable and are for illustrative purposes only Ezetimibe 10 mg daily. Repatha® monotherapy: Repatha® 140 mg bi-weekly. Bempedoic acid fixed-dose combination. 180 mg Bempedoic Acid/10mg Ezetimibe
*In the FOURIER trial, 59% LDL-C reduction was achieved with Repatha® in addition to high- or moderate-intensity statin therapy.
-
Meet Zara
-
Further Data - Zara
Case Study

Newly-diagnosed HeFH with one cardiovascular event
LDL-C 3.9 mmol/L currently treated with atorvastatin 40mg
ESC/EAS target 1.4 mmol/L AND ≥50% reduction from baseline;1
NICE PCSK9i eligibility threshold ≥3.5 mmol/L2
NICE lipid target: 2.0 mmol/L or less3
Case Study
Potential LDL-C reductions from baseline
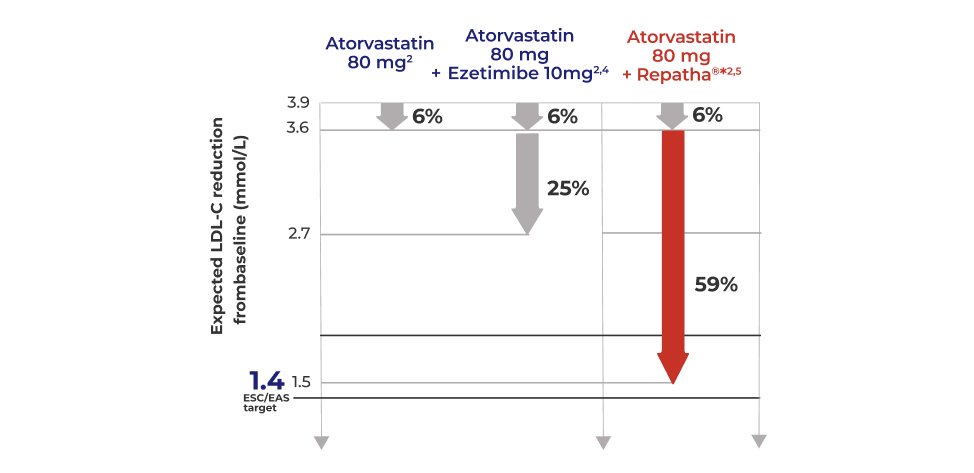
The expected LDL-C reduction and LDL-C levels between treatment regimens are not comparable and are for illustrative purposes only. High intensity statin: atorvastatin 40mg or 80mg daily. Ezetimibe monotherapy: Ezetimibe 10 mg daily. High intensity statin monotherapy and ezetimibe: Atorvastatin 40mg or 80mg daily, and ezetimibe 10 mg daily. Repatha® monotherapy: Repatha® 140 mg bi-weekly.
*In the FOURIER trial, 59% LDL-C reduction was achieved with Repatha® in addition to high-or moderate-intensity statin therapy.
-
Overview
-
Transcript
In this short video, Professor Dev Datta (Consultant in Metabolic Medicine, Cardiff) and Professor Azfar Zaman (Consultant Interventional Cardiologist, Newcastle) explore the therapeutic options for managing Sue’s case, including guideline-recommended lipid targets, and the potential benefits of adding lipid- lowering injectables to her regimen.
Azfar Zaman:
My name is Azfar Zaman. I'm an Interventional Cardiologist Clinical Professor of cardiology at Newcastle upon Tyne Freeman Hospital. It's a pleasure to introduce my co-chair, Dev Datta.
Dev Datta:
Thanks, Azfar. So my name is Dev Datta, I'm a consultant in metabolic medicine in Cardiff and Professor of Preventive Cardiovascular Medicine at the University of South Wales.
Dev Datta:
Sue, somebody who I'm sure will be familiar in your clinical practice, Azfar. So she's a retired teacher. She's now 68. She's got a background history of hypertension, and she was diagnosed with peripheral arterial disease just over a year ago. But she's also now sustained a myocardial infarction fairly recently, just two months ago. We identify that she's got a body mass index of 35, and looking at her lipid profile, she's got a total cholesterol of 5.9 an HDL cholesterol of 1.4 an LDL cholesterol of 3.9, normal triglycerides at 1.4, blood pressure of 138/88. In terms of medication, she's taking a beta-blocker, an ACE inhibitor, a calcium channel blocker, proton pump inhibitor and dual antiplatelet therapy following her intervention. With regards to her lipids, she's taking Atorvastatin 80 mg once daily as well as Ezetimibe 10 mg once daily. And the Atorvastatin has been increased from 40 mg once daily which is what she was taking prior to the event that she sustained. So I'm interested is this enough?
Azfar Zaman: Yes, I mean, she's very typical of the type of patients that we will see. The first thing to state is that she's had an admission with an acute coronary syndrome, and we know that these patients have a one in five, 20% chance of a recurrent ischemic event in the first 12 months (Hemingway H, ESC Oral Presentation, 2014; Jernberg T et al, 2015). So Sue is at high-risk of recurrent events, and it is imperative that we not only control the risk factors such as hypertension, but you see the total cholesterol, the non-HDL cholesterol, all of these are way above what the recommended guidelines are (NHS, 2022). So in answer to your question, Dev, yes, this is the typical patients that we see. She's on standard, what I call first generation secondary prevention medication. But there is a lot more that we can and indeed should do to manage this patient's risk profile.
Dev Datta: I guess should we just be adding in additional oral therapy here, noting that she's already on Ezetimibe, it's going to be quite difficult, isn't it to add in additional oral therapy here to try and get her to levels that we would consider appropriate. So what do we think in terms of next steps?
Azfar Zaman:
I mean, it's a really good question and one of the points that I want to get across to people listening is how much more aggressive the European Society guidelines are for risk-based LDL cholesterol goals. We now have to achieve either a 50% reduction from baseline or to achieve an LDL cholesterol goal of less than 1.8 mmol/L. If patients are deemed to be at very high risk, then we either have a 50% reduction from baseline or achieve, and rather, achieve, LDL cholesterol target of less than 1.4 mmol/L (Mach F et al, 2020). So these are aggressive targets. So the question that I always have in my daily practice is owe see levels such as this, should we be initiating injectables or further treatment?
Dev Datta:
Certainly we understand that early intervention is helpful. I might refer to the open-label extension study for FOURIER which looked at the patients who were initially treated with placebo compared to the patients who were initially treated with Repatha right at the beginning of FOURIER and then you’ve got 2.2 years later and then offering them all open-label Repatha (O’Donoghue ML et al, 2022; Sabatine MS et al, 2017). What I find interesting is that if we look then five years beyond into the open-label extension, the patients who were initially randomised to Repatha had favourable outcomes (O’Donoghue ML et al, 2022). If you've got a patient like Sue who's already on fairly reasonable oral therapy, I'd be quite keen to initiate an injectable such as Repatha at an early stage and ideally at admission.
Azfar Zaman:
If we come back to Sue and put her in that risk category, you know, moderate, high or very-high, there's no doubt that with her MI two months ago, with diagnosed peripheral arterial disease and hypertension, she fulfils that criteria of very-high-risk (Mach F et al, 2020). So whether you look at NICE criteria which for very-high-risk is 3.5 mmol/L of LDL cholesterol (NICE, TA394), or indeed you go to the much more aggressive ESC targets, it is almost certain that we will need to start Sue on an injectable such as Repatha at the two-, three-month mark.
Dev Datta:
Absolutely. I'm just thinking now in your experience from the cardiology space, thinking about practical issues about getting our patients to target, I mean, do you think we'll get there with Sue because her LDL's pretty high. Are we going to be able to get there with Repatha or any medicine noting where her LDL is now?
Azfar Zaman:
So if we go back to the FOURIER trial, we know, and from previous studies with Repatha that we can expect a 59 to 60% reduction in LDL-C within the first four weeks (Sabatine MS et al, 2017). So we may not be able to get to the less than 1.4, but we will get her to below certainly 2.6, which is the advice level for moderate risk. So I think my feeling would be for this patient that we would start her on Repatha at the three month mark, repeat after a month and make that assessment once again as to whether she would need additional therapy.
Azfar Zaman:
I think at this point though, it would be worthwhile talking about the tolerability of these agents. So certainly in cardiology we've not been used to giving or prescribing injectables for our patients. We have been a very oral-based specialty. We've had to educate patients about injectables. And then we've had to reinforce the fact that these agents are working. In our experience, the tolerability has been well, what I will say, it's reflected in what we've seen from clinical trials.
Dev Datta:
Absolutely. The incidence of side effects being consistent with that seen in FOURIER, having injection sites reactions and sometimes nasopharyngitis (Sabatine MS et al, 2017). But these tend to be self-limiting. And I think if we look at the patients who we initiate on injectable therapies and when we review them 1, 2, 5 plus years down the line, it's reassuring to note longer term adherence to therapy.
Azfar Zaman:
Now I think it is worth stating also that whilst LDL cholesterol is one important risk factor, in this particular case for Sue, there are other risk factors that we should not ignore. Namely, you know, the hypertension, the BMI, her sedentary lifestyle (NICE, MI – secondary prevention). So there are many risk factors that need to be addressed and I recognise Sue, I know this is a fictional case, but I recognise Sue.
Azfar Zaman:
We have to recognise that there has been a change in the guidelines which leads us to be more aggressive in management of LDL cholesterol. Second, that there are multiple pathophysiological mechanisms for coronary artery disease, and we should try and address as many of these as possible to prevent future events (Quality and outcomes framework guidance, 2024/25). But addressing cholesterol has become easier for clinicians because we now have a multiple array of agents, including Repatha and other injectables, including other oral agents on top of statins and Ezetimibe, which can help us to achieve those goals.
Azfar Zaman:
So thanks very much, Dev, that was educational for me, educational, I hope for our listeners.
Dev Datta:
That’s great. Thanks very much, Azfar.
*these are fictional case studies for illustrative purposes only.
Abbreviations
EAS, European Atherosclerosis Society; ESC, European Society of Cardiology; FDC, fixed-dose combination;
HeFH, heterozygous familial hypercholesterolaemia; LDL-C, low-density lipoprotein cholesterol; NICE, National Institute for Health and Care Excellence; PCSK9, proprotein convertase subtilisin/kexin type 9.
-
References
- Mach et al., European Heart Journal. 2020; 41: 111-88.
- https://www.england.nhs.uk/aac/publication/summary-of-national-guidance-for-lipid-management/ Accessed April 2025
- Cardiovascular disease: risk assessment and reduction, including lipid modification: https://www.nice.org.uk/guidance/ng238/chapter/Recommendations/ Accessed April 2025
- Ezetimibe Summary of Product Characteristics.
- Repatha® (evolocumab) Summary of Product Characteristics.
- Pander et al., J Intern Med. 2009; 265(5): 568-80.
- Nustendi® Summary of Product Characteristics.
-
Adverse Event Reporting InformationAdverse events should be reported. Reporting forms and information can be found at www.mhra.gov.uk/yellowcard or search for MHRA Yellow Card in the Google Play or Apple App Store. Adverse events should also be reported to Amgen Limited on +44 (0) 1223 436441.



